Table of Contents
Baseline study - implementing the Passive House concept in hospitals
Below you find a summary of the Baseline study - implementing the Passive House concept in hospitals. It was conducted under behlaf of the Ministry of Economic Affairs, Energy, Transport, and Housingfor the State of Hesse.
The full study can be downloaded here.
Please note: The download links will take you to the Passive House Portal, where you need to login in order to access the report. Login details to the database may differ from your membership login details to Passipedia. Please sign up to the Passive House Portal in case you don't yet have an account. Registration to the Passive House Portal is free and can be canceled at any time. In case of questions contact info@passivehouse-international.org
The guide was developed in the German context and then translated into English. Therefore, the translation may not take into account international or country-specific construction aspects and regulations.
Introduction
Evaluations of consumption statistics show that hospitals are among the buildings that consume the most energy. A lot of the 2,080 hospitals in Germany with a total of 503,422 beds [Destatis 2009] need to be renovated. To evaluate and tap the conservation potential of retrofits and energy-efficient new builds, the State of Hesse studied basic issues for the implementation of the Passive House Standard in hospitals while constructing a new build for the Frankfurt Höchst Clinic [Schumacher/Kah 2012, Naß/Frydrychowski 2013]. This paper presents the main insights from the baseline study [Kah et al. 2013].
It is often assumed that the Passive House Standard only concerns demand for heating energy. But the goal in hospitals is to considerably reduce the amount of energy used by all healthcare applications while maintaining at least the same level of comfort. As has already been done with other non-residential buildings (such as educational facilities and swimming pools), the first step in studying hospitals is to identify all energy consumers and determine what the usual consumption values are and what the savings potential is. Within a building, energy flows are not unrelated; for instance, efficient devices can reduce the demand for cooling. The influence of different applications becomes more relevant the more efficient the building is. Conventional energy balances, such as DIN V 18599, do not, however, take account of functional energy applications, such as medical devices.
Special aspects of hospitals
When it comes to implementing the Passive House concept, a few special aspects of hospitals must be taken into consideration, including areas with sensitive hygiene requirements, elevated comfort requirements for recovering patients and the elderly, the wide range of various energy applications, and processes that give off great amounts of waste heat within the given area.
An analysis of guidelines shows that the use of tried and tested energy-saving technologies faces no obstacles in principle. Indeed, hygiene and energy efforts sometimes complement each other. High-quality insulation on potable water lines and optimized taps (in accordance with RKI 1) used only where water is frequently needed reduce the risk of Legionella's disease even as it lowers distribution losses in drinking water lines. If there are special requirements for areas where hygiene is of utmost importance, such as operating rooms, the solutions must be adjusted accordingly. New concepts and approaches should always be coordinated with hygiene experts and hospital management as early in the process as possible.
In rooms where medical care is provided, the greatest comfort is at room temperatures between 22 and 23 °C. For patients not wearing a lot (such as when they are washed in bed), room temperatures should be higher. In addition, the wide range of energy applications depends on the type of clinic. The Baseline study on implementing the Passive House concept in hospitals investigates those most relevant for energy.
Often, the question is whether efforts to reduce heat demand are worthwhile if there is so much waste heat from processes within the hospital anyway. A closer analysis of processes that use low-temperature waste heat shows that the additional processes needed to recover that heat would reduce the benefits, in terms of primary energy, to just a fraction. The use of waste heat from inefficient processes and devices is a good idea and should be investigated, but not before the processes producing the waste heat in the first place have been optimized.
Hospitals generally require 24-7 operation and have special demands for thermal comfort. Insulation therefore pays off quickly. Even in conventional hospitals, indoor air ventilators are commonly used. It is therefore only a small step to controlled ventilation with heat recovery throughout the building. Hospitals are thus good places to apply the Passive House concept.
Energy applications in hospitals
A particular clinic's equipment depends on its specific focus, and it considerably affects energy demand. Consumption differs considerably depending on whether the clinic sterilizes its own instruments, has its own cafeteria, washes its own laundry, and conducts medical imaging.
The investigation shows that it pays to take a look at use-specific energy applications not taken into account in conventional energy balances, such as DIN V 18599. These processes become more important as the building envelope and building services become more energy efficient. The applications not taken into account in conventional energy balances make up nearly 50 percent of total primary energy demand in Passive House buildings. Yet, there is considerable efficiency potential in such energy applications. Currently available devices and improved processes can reduce energy consumption by more than 30 percent even though energy efficiency has not been a focal point for medical and professional appliances the way it has been for household appliances. Figure 1 shows the share of primary energy demand from large appliances in a clinic when that focuses on energy efficiency based on the example of the planned new building at the Frankfurt Höchst Clinic.
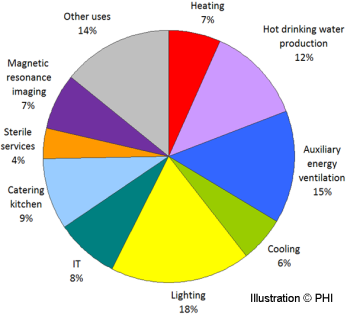 |
| Figure 1: The share of different energy applications in primary energy demand based on the planned new build for the Frankfurt Höchst Clinic. |
Hospitals have a wide range of processes and devices. Comprehensive energy savings will probably only truly be possible if such products also have energy labels. It is unrealistic to expect planners to look into which devices and applications are available on the market and for engineers to estimate their energy demand.
The investigations also show that heat demand can be reduced by 60 percent and final energy demand by 50 percent (compared to a conventional new build) if heating, ventilation, hot water, and auxiliary energy are made more efficient.
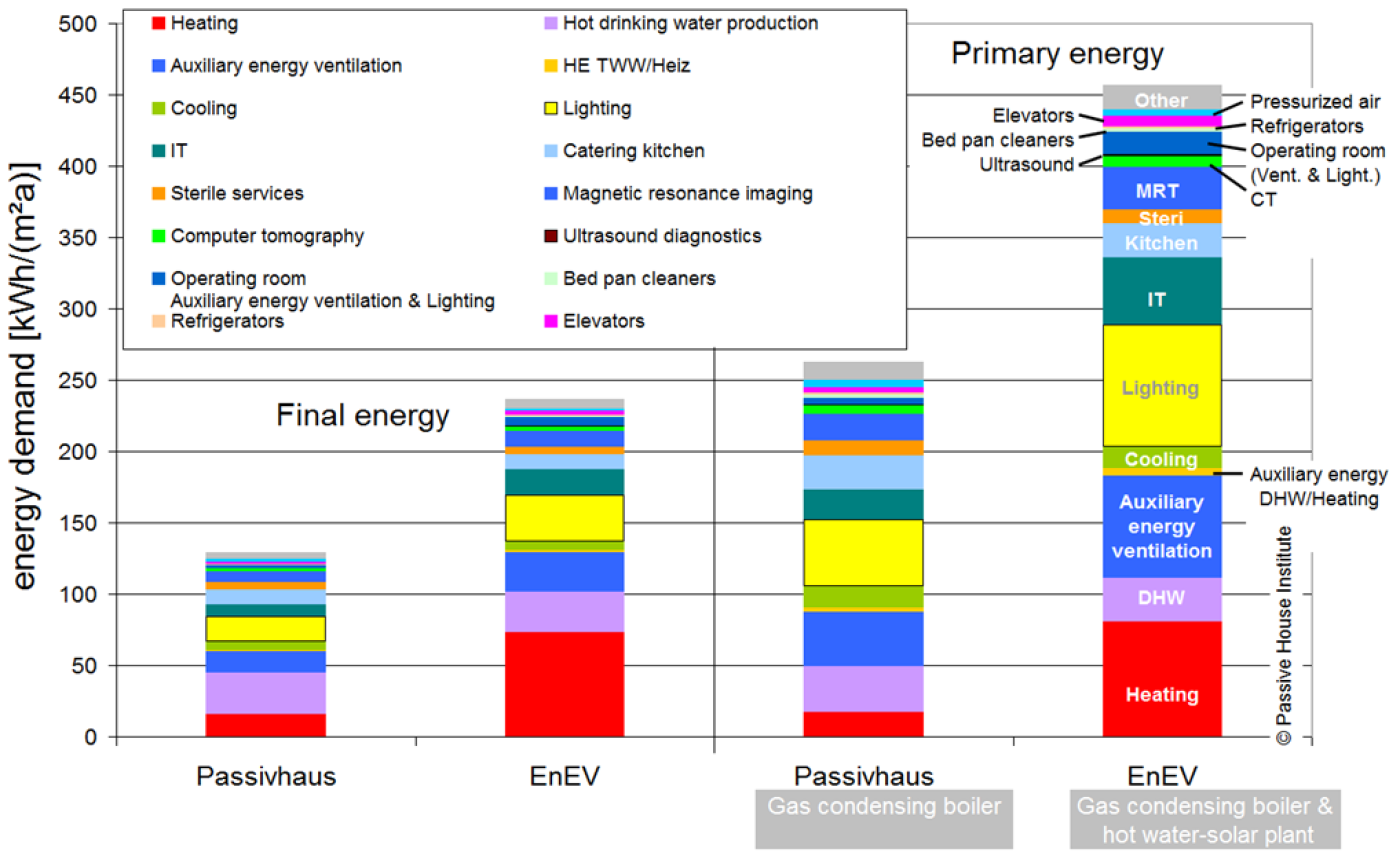 |
| Figure 2: Example of energy demand values from all energy applications in a hospital (EnEV: reference in accordance with the German EnEV 2009). The Passive House variant is based on rather conservative assumptions of improved efficiency [Kah et al 2013]. |
In terms of primary energy demand for all applications in a hospital providing maximum care, the savings from the use of available technologies of greater efficiency come in at 40 to 50 percent. In Figure 2, the results are presented for selected energy applications.
Heating
Hospitals are generally large, compact buildings. The Baseline study - implementing the Passive House concept in hospitals shows that the use of efficient technologies can, with reasonable effort, reduce heating demand to 15 kWh/(m²a) even though target indoor temperatures and air exchange rates are greater than in other buildings.
As in other Passive House buildings, good insulation means that the type of heat distribution does not matter much. Still, for various reasons, it is more practical to use surface heating systems in hospitals so that ventilation and heat run separately. Synergies can occur, for instance, when radiators are used for both heating and cooling.
All standard supply solutions are possible. Cogeneration is an interesting solution because of the large constant demand for hot drinking water and electricity.
Hot drinking water
The main ways to reduce energy demand for hot drinking water are to use water-saving fixtures, reduce distribution losses, and make water heating more efficient.
Forecasts of energy demand and energy-focused optimizations for hot drinking water should be based on realistic consumption values. If no data are available (no existing building with comparable supply level), 50 liters per bed per day can be used as an average (based on the literature and the authors' own measurements).
Up to 50 percent of demand for hot water supply is heat lost in distribution lines. Efforts to reduce heat losses simultaneously reduce undesired heat transfer to cold water lines and help reduce internal loads in the summer. The hot water network should therefore be as compact as possible and insulated above and beyond what's required by EnEV [Kah et al 2014].
Optimized supply lines and greater insulation reduced distribution losses by 33 percent below the level of a conventional central distribution system with pipes insulated in accordance with EnEV 2009. Carbon emissions from hot water supply can be further reduced if renewable energy is used (such as solar thermal). Using waste heat to preheat potable water is another interesting option.
Cooling
The focus should first be on reducing all cooling loads, including greater efficiency of artificial lighting, IT, and medical devices. Shading is crucial to reduce solar loads. Sufficiently accessible storage mass, such as unclad concrete ceilings, buffer summer temperature peaks, improve the building's climate in the summer, and serve as the basis for passive cooling; the building itself is used to store excess heat, which it then gives off at night.
If energy-efficient applications are consistently used, internal loads will remain modest, and when exactly they occur will not play such a major role if the building has enough storage mass. Passive cooling largely suffices to ensure summer comfort.
Cooling based on large volumes of conditioned air far beyond the flows required for hygiene should not be used unless such passive measures as storage mass cooling do not suffice.
Ventilation
In the functional areas of a hospital – such as operating rooms, intensive care, and laboratories – controlled ventilation with high-quality filtering is essential. But even in other areas, especially where medical care is provided, controlled ventilation should still be provided to ensure good air quality over the long run.
Even if the ventilation systems are energy-efficient, auxiliary power for those systems constitutes a large share of a hospital's total energy demand. [Bräunlich 2014] takes a closer look at the following aspects for the planning of energy-efficient ventilation:
- Adapting air volumes to actual demand (dimensioning and controls)
- Low pressure losses in the ducts; pressure losses per tract should not exceed 200 Pa, for instance, for functional areas with low requirements for air supply (such as care stations)
- Energy-efficient ventilators (specific power consumption should not exceed 0.45 Wh/m³)
Lighting
Hospitals generally have longer operating times than other non-residential buildings. Many parts of hospitals are also used on the weekend and at night.
Wards and hallways where general care is provided have the highest energy demand because they are used all the time, as calculations of the need for artificial light show. While the minimum illumination requirements are the greatest in examination and medical rooms, day-lighting also helps the most there because such activities mainly take place during the day. Demand for artificial light is therefore much lower there than in the wards.
Furthermore, calculations show that energy demand can be reduced considerably below the assumptions in EnEV 2009. The main progress comes from efficient artificial lighting, which reduces energy consumption by 70 percent in wards and by 60 percent in examination and medical rooms if the lighting equipment is optimal (compliance with SIA 380-4).
In wards, integrated lighting solutions are often installed in supply rails. Such modular system lighting fulfils healthcare demands and creates a pleasant atmosphere. The indirect general lighting does not, however, fulfill the recommended electrical target values, even if LED lights are used.
Central sterilized goods department
The sterilization department is another area of major consumption in hospitals. The cleaning and subsequent sterilization processes for operating utensils and other sterile goods play the biggest role in terms of energy.
Most of the energy used by cleaning and disinfection machines goes to heating water. That is therefore where the most energy can be saved, as well. Water can be conserved by adapting water volumes to the duration of soaking before rinsing and the kind of utensils to be cleaned; in this way, around 20 percent of the energy used in the cleaning process can be saved.
Most of the energy input (more than 60 percent) goes into the waste water as heat after cleaning. Heat recovery systems integrated in cleaning appliances – a common feature of commercial dishwashers – are not offered for sterilized goods cleaning machines. Tanks that at least reuse hot distilled water (93 °C) from the disinfection phase are an interesting solution.
Steam sterilization is the safest but most energy-intensive process – and the one preferred in various guidelines for hospitals [KRINKO 2012]. In this process, pure, saturated water vapour is used to sterilize the surface of utensils.
Due to the process up to 70 percent of the energy is transferred to the cooling water in cyclical vacuum and steam injection phases (in the condenser and via the pump).
Considerable amounts of heat escape into the warm wastewater during the cleaning process and into the vacuum facility's cooling circuit during steam sterilization. At least some of it could be used in other processes, such as potable water heating, if proper technical solutions are used.
Magnetic resonance imaging (MRI)
Full-body systems used today generally have magnetic fields of 1 to 1.5 teslas, though the latest systems go up to 3 teslas. Super-cooled superconducting coils generate these strong magnetic fields. The constant cooling required – near zero Kelvin – accounts for a large share of energy consumption for MRIs.
And because this cooling is constant, the power load is as well. In contrast, processes during the actual imaging cycle do not last long and are of less importance.
Here, shortening the imaging process could help reduce energy consumption, particularly by allowing the same number of diagnoses to be provided by fewer MRI systems. The same goes for longer operating times, which would also allow fewer systems to handle the same demand.
Some units are also thriftier than others, though manufacturers do not yet provide standardized energy labels, which would facilitate comparisons – and help formulate specifications in requests for proposals. There is also further potential in the more efficient cooling of the MRI by the building.
New superconducting materials would also reduce consumption considerably if the superconducting effect could occur at higher temperatures and no helium cooling were needed.
Summary
If everyone involved takes part in the process from the outset (including medical technology planners), integrated planning can contribute to a project's success considerably, especially in the case of complex hospitals. Specific investigations of individual items in advance prevent subsequent iteration and present solutions that are optimized in terms of energy and cost.
This study showed that it pays to take a look at use-specific energy applications not taken into account in conventional energy balances, such as DIN V 18599. These processes become more important as the building envelope and building services become more energy efficient. A hospital's equipment has a major impact on resulting energy demand. Demand was determined based on a hospital providing maximum care, but it can only be a generalization. Efficient technologies already available can reduce primary energy consumption across all applications by 40 to 50 percent below the level of a conventional new building.
Supply solutions that take advantage of ambient energy or are based on renewables are additional ways of reducing primary energy demand for heat supply. In a Passive House hospital, however, efficiency measures already minimize heat demand, so the use of renewables and efficient heat pump systems will only have a limited effect on total energy demand.
In addition, there are no proper energy demand labels for many hospital devices. Even if energy-efficient appliances are to be used, it is almost impossible to compare products and specify energy quality in requests for proposals – even for medical refrigerators. Complicated certification procedures for medical devices also slow down the optimization of devices.
References
[Bräunlich 2014] K. Bräunlich, O. Kah, Aspekte einer effizienten Lüftung in Krankenhäusern / Aspects of efficient ventilation in hospitals, 18. PHT 2014 Aachen.
[Destatis 2009] Statistisches Bundesamt, Stand 2009
[Kah et al 2013] O. Kah, K. Bräunlich, T. Schulz, A. Grill, O. Ottinger, R. Schumacher, Grundlagenstudie zur Umsetzung des Passivhauskonzept in Krankenhäusern / Baseline study on implementing the Passive House concept in hospitals, Studie im Auftrag des Hessischen Ministeriums für Wirtschaft, Verkehr und Landesentwicklung, Passivhaus Institut, Darmstadt 2013.
[KRINKO 2012] Anforderung an die Hygiene bei der Aufbereitung von Medizinprodukten, Empfehlung der Kommission für Krankenhaushygiene und Infektionsprävention (KRINKO) beim Robert Koch-Institut, Bundesgesundheitsblatt 2012 55: 1244-1310.
[Naß / Frydrychowski 2013] W. Naß, J. Frydrychowski-Horvatin, Das erste Passivhauskrankenhaus Deutschlands – eine Herausforderung, der sich die Stadt Frankfurt gerne stellt! / The first Passive House hospital in Germany – a challenge that the City of Frankfurt is pleased to take on, 17. PHT 2013 Frankfurt.
[RKI 1] Robert Koch Institut, Richtlinie für Krankenhaushygiene und Infektionsprävention, (Alte Anlagen der Richtlinie für Krankenhaushygiene und Infektionsprävention)
[Schumacher / Kah 2012] R. Schumacher, O. Kah, Grundlagenstudie - Umsetzung des Passivhauskonzept in Krankenhäusern / Passive House hospitals - boundary conditions for the design, 16. PHT 2012 Hannover.
[SIA 380-4] SIA 380-4, Ausgabe 2006: Elektrische Energie im Hochbau, Schweizerischer Ingenieur- und Architektenverein, Zürich
See also
Overview of all articles on Passipedia about non-residential Passive House buildings
Overview of all articles on Passipedia about hospitals
Click here to read more about the Guides and Aids
List of all released conference proceedings of the 18th International Passive House Conference 2014 in Aachen
Conference proceedings 18th International Passive House Conference 2014
